Category: WLS
Optimizing Pre-operative Health Status
November 12, 2014 1:23 pm
- Maintaining a healthy diet
- Cessation of ALL tobacco and alcohol use
- Do not use NSAIDS prior to surgery or after surgery until cleared by surgeon
- Getting plenty of rest
- Staying Hydrated
- Pulmonary embolus prevention exercises such as ankle circles and point and flex toes
- Maintaining or starting a regular activity level. Any amount of increase in activity will benefit you after surgery. Walking, squats, lifting weights with arms
- Full laboratory blood studies and vitamin levels as ordered by the surgeon
- Start and optimize your vitamins, calcium and other mineral and supplements. Vitamin D deficiency increases surgical complications. (Another Vitamin D article)
- Manage preexisting health conditions (diabetes, sleep apnea, high blood pressure etc..) Follow instruction in regards to what medication to stop or continue before surgery i.e. Aspirin, blood thinners, medications that interfere/interact with anesthesia, etc.
- Two forms of Birth Control if indicated.
Mental preparation:
- Have a clear understanding of the procedure
- Study all information provided to you regarding your surgery
- Remember that surgery is one of many tools to assist in weight loss and improved health. It does not fix other issues.
- Realistic expectation of the outcome of surgery
- The role of family involvement for support
- Be prepared with all the purchases for the post operative diet, vitamin and mineral supplements.
- There is also a number of other variables that will improve the long term outcome of the weight loss surgery:
- Investigate Protein Supplements for the highest bioavailability
- Try and eat whole, unprocessed foods
- Read labels on all food items
- Look for high protein recipes
- Network with supportive people who will provide a positive influence
- Long term success also depends on:
- Maintain daily protein requirements
- Maintain daily vitamins, calcium, minerals and other supplements
- Routine follow up with your bariatric surgeon.
- Routine laboratory studies to surveil vitamin and mineral levels.
- Get your medical advice from your surgeon.
- Get suggestions from other patients. Do not confuse this with medical advice.
Patch or Spray Vitamins
August 15, 2014 10:37 pm
At the last group meeting, there were several questions whether vitamin D and other vitamins would be absorbed via patch (transdermal) and spray (buccal/sublingual) routes. After reviewing several resources, the only article I could find was for transdermal Vitamin D absorption. However, if we look at the mechanism for each route we can make an educated assumption.
Transdermal route of absorption (without additional absorption enhancers) (ref) requires a molecular mass less than 500 g/mole, high lipophilicity (affinity to fat or lipids), and low required daily dose (less than 2mg). The fat-soluble vitamins are definitely lipophilic, all of them have molecular weights less than 500 g/mole and daily dose is under 2mg. It seems that hydrophilic medications (that have an affinity to water) may have less ability to be absorbed with this route unless a chemical enhancer is added to the product. Most vitamins and minerals have lower molecular weights except Vitamin B12 which has too high of a molecular weight unless an enhancer is added. The transdermal route has slower absorption than buccal (oral mucosa) but faster than usual tablet oral route. The down side to transdermal route is possible skin issues due to medication, adhesives, and also different rates of absorption due to skin thickness and condition.
Buccal/sublingual route of absorption is dependent on lipid solubility, oil to water partition coeffincient, saliva pH, small to moderate molecular weight, and oral mucosa thickness. The mechanism of action is osmosis, which means items that readily dissolve in water are easily absorbed. Unlike orally ingested medicates, that take time to absorb and need to be filtered and/or processed in the liver, sublingual route is fast absorbing and the liver is bypassed. The down side to this route is it disrupts eating and drinking and is not efficient with smoking due to vasoconstriction.
An e-mail was sent to the companies inquiring about the outcomes of their products with people with malabsorption issues. No response was received from the spray vitamin companies.A request was also sent to obtain any research articles they may have but a response has not been received at this time. The following is the response I received from the maker of Patch MD.
“I am the president and founder of Patch MD. We design Patch MD to help people that have digestive issues and malabsorption. Our whole premise is to avoid the digestive track, by doing so we avoid dealing with conditions such as short bowel syndrome, acid reflux, and bariatric surgery to name a few. People also with Crohn’s disease and iliac disease are challenged with digestion and absorption every day of their life. Our patches are designed specifically to pass nutrition through the skin into the bloodstream. We get letters every day from people that have had bariatric surgery and were unable to get vitamin D, calcium, the B’s and Vitamin A and K, our product works because we use the skin as our delivery system, absorption is through the skin, avoiding all digestive potential issues. The only problem that we may have is we tell our customers to use no lotions or cream in the patch application area, as you may understand it will prevent absorption. We are going to be at a national convention this weekend in Manhattan Beach California to take part and display our products at the ObesityHelp conference. They ask us to take part as they were getting great reviews from their members that are using the patch. All were improving their blood work after taking Patch MD patches.”
Earl Hailey, President Patch MD
In light of the review of data, it would seem that the transdermal route would be beneficial to people who are having issues maintaining blood levels of fat-soluble vitamin levels. The other vitamins also have a good prospect of absorption via transdermal route. Buccal or sublingual (sprays) would seem to have a better outcome for water-soluble vitamins unless there is an additive added to the product to increase the solubility of the fat-soluble vitamins and make them water miscible. We must realize that there is no data for Duodenal Switch patients and very little data regarding these routes of absorption with vitamins specifically. If you are going to try these types of vitamins you should be extremely diligent in following your laboratory studies for vitamin levels with greater frequency until it is determined they are maintaining your blood levels.
Also, it should be noted that water miscible (dry) Vitamin A, D, E, K are the only type of these vitamins a DS patients should be taking. Over the counter Vitamin A, D, E, K are fat-soluble and due to the fat malabsorption after DS these type of vitamins are not appropriate to maintain blood levels. Water miscible (dry) vitamins should NOT be taken with fatty or oily foods and should also be taken 30 minutes prior or 30 minutes after eating. The water miscibility makes them water soluble and therefore will not have optimal absorption if taken with fat. Fat also increases the rate of digestion through the small bowel after DS and decreases the amount of time the vitamin has in the bowel and therefore, decreases absorption. They are best absorbed when taken on their own.
The good news patches and spray routes of administering medications and supplements is an up and coming area of research. There are several ongoing research studies and new developments on the horizon for increasing absorbability of transdermal route with different types of additives and techniques.
Protein Malnutrition Protein Part 2
July 31, 2014 1:25 pm
Protein energy malnutrition (PEM) or Protein Malnutrition is a problem that can effect a few after weight loss surgery (WLS) and Duodenal Switch (DS). In our previous blog post on protein we discussed the types of essential and non-essential Amino Acids and possible sources. We also discussed how to choose the best bioavailable protein and to vary protein sources to achieve adequate protein levels. There are cases even with adequate protein intake that can result in PEM due to inadequate protein absorption. The early signs of low protein may be low energy, muscle weakness, moodiness, inability to sleep well, joint pain, changes in hair and nails and carb craving. It is imperative after WLS that you maintain your protein levels throughout your lifetime. The minimum protein intake is 80-100 grams per day after WLS. There is no leeway where protein is concerned. It is important in almost ever function in the body.
There are two types of protein energy malnutrition, Kwashiorkor and Marasmus:
Kwashiorkor is a lack of protein intake with adequate or slightly lower caloric intake. It’s symptoms are edema (swelling in legs, ankles, feet) enlarged abdomen, irritability, anorexia, hair discoloration and loss, muscle weakness, changes in psychomotor function, mental lethargy, ulcerations, brittle nails, rash or discoloration of the skin, bradycardia (slow heart rate), non-tender parotid enlargement, enlarged liver with fatty infiltrates that are similar to alcohol liver disease. The edema is caused by osmotic imbalance in the intestinal system causing swelling of the gut. Protein, primarily albumin is responsible for the colloidal pressure within the circulatory and tissue systems. The lack of protein within the circulatory systems cause fluids to “leak” into tissues causing edema. Gastro-intestinal symptoms can include nausea, vomiting, dehydration, diarrhea and increases in appetite. People who have pathological bacteria or parasites and/or after WLS diarrhea can precipitate lower levels of protein. If left untreated can lead to protein malnutrition.
Marasmus is characterized by a lack of protein and caloric intake. The symptoms are an emaciated appearance with edema. There is no liver changes as in Kwashiorkor. This is a starvation mode and can be difficult to treat and can progress to a point of no return.
Catabolysis is the bodies response to lack of protein and or nutrition. This biologic process breaks down muscle and fat to maintain bodily functions. Catabolysis is the body’s last resort to keep it alive. It is a starving body eating itself to keep vital organs alive.
Laboratory Studies are needed to determine the level of malnutrition and treatment routes. These studies include:
- Lipids
- CBC (complete blood count)
- CMP (comprehensive metabolic panel) includes liver and kidney function tests, Calcium and electrolytes
- Albumin Normal is greater than 3.5 gdL (transports nutrients such as calcium, zinc and Vitamin B6)
- Prealbumin (transthyretin) transports retinol (Vitamin A)
- Total protein Normal is greater than 6.3 gdL
- Iron tests such as serum iron, TIBC, and ferritin
- Vitamins and trace minerals such as B12 and folate, vitamin A, vitamin D, vitamin K, B vitamins, calcium, and magnesium
- Ova and Parasite stool testing
Protein is an extremely important nutrient within our bodies and is considered the workhorse in cells and organs. They are responsible for catalysts, messenger duties, structural, immunoprotectors, transporters, buffers, fluid balancers and many other roles. Protein has a hand in synthesizing other proteins, regulates protein turnover, enzyme activity, neurotransmission, gene transcription, transport of other nutrients, messenger and signals for growth hormone and insulin, structure, storage for other nutrients and immunity.
The muscular system is the most obvious structural protein in our bodies, 40% of the total body protein, as is hair, fingernails and cells. Our organs also require protein in order to function appropriately. However, protein’s role in red blood cell formation, size and health is extremely important. If you don’t have adequate protein levels your body can not make red blood cells. Transferrin is a protein that carries iron to receptors. Ferritin is an intercellular protein that stores iron until it is needed. Glycine is a protein for heme synthesis. B12 is also transported via a protein for red blood cell production. Protein is also important in blood clotting and plasma.
Cardiovascular health is also reliant on protein for structure and function. Also, proteins can have a protective effect at the mitochondrial level.
Kidney function relies on protein to regulate the acid base balance and ammonia disposal. The kidneys are also the site of amino acid production.
Protein is also important in bone health as a carrier for Vitamin K and calcium binding, tissue repair, healing and growth. Proteoglycans play a role in extracellular structures such as skin, bone, and cartilage. Also related to the skeletal system are glycoproteins, which also aid in building connective tissue, collagen, elastin and bone matrix.
Central Nervous system relies on proteins for neurotransmission, hormone production and other functions. Protein deficients can lead to neurologic problems such as altered behavior and mental function among other manifestations. The neuorpeptides have actions on transmission functions, mood and behavior. They can also effect a wide range of functions such as blood pressure, body temperature, pain sensation, and learning ability.
Immonoproteins are the group of proteins that provide immune protection such as immunoglobulins and antibodies.
Protein also have storage roles for copper, iron and zinc called metalloproteins. Copper and zinc are considered neurotransmitters, important for iron metabolism, and connective tissue formation in heart, blood vessels and skeletal.
There are situation where your protein needs will increase. In cases of wounds, burns, surgery, stress, sepsis or other illnesses, protein requirements increase. Also age, pregnancy, lactating and increased exercise increases protein needs.
Protein Energy Malnutrition is protein deficit that can and should be avoided after WLS. PEM, if left untreated, can lead to organ failure and death. Protein is crucial in almost every function of the body and without adequate levels there will be symptoms and side effects. Please take care to maintain your protein levels throughout your life. We have discussed several of protein’s function, however, there are many more.
Phytates the anti-nutrient?
June 20, 2014 3:33 pm
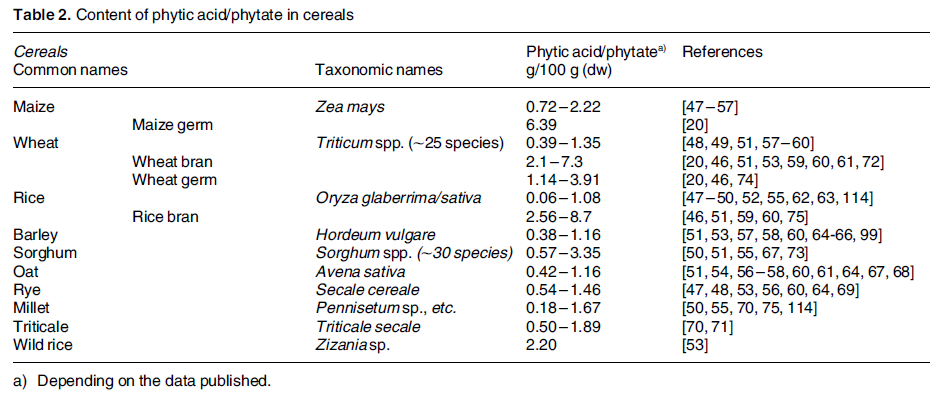
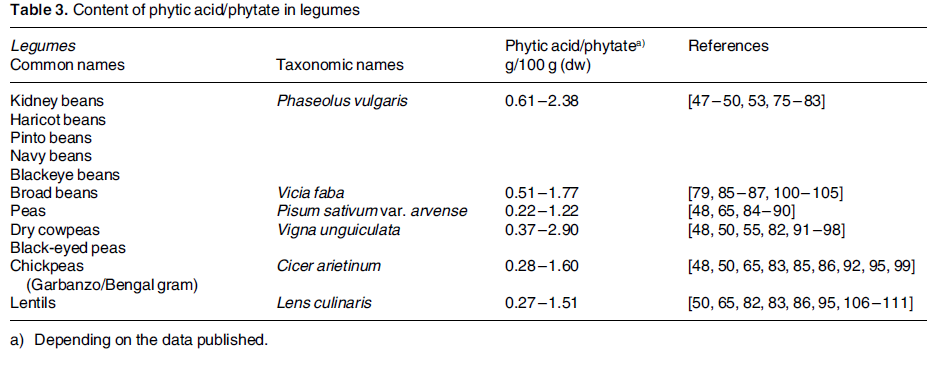
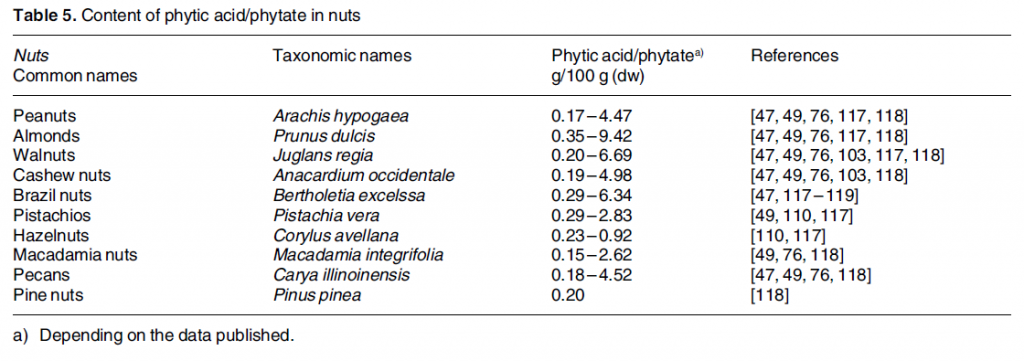
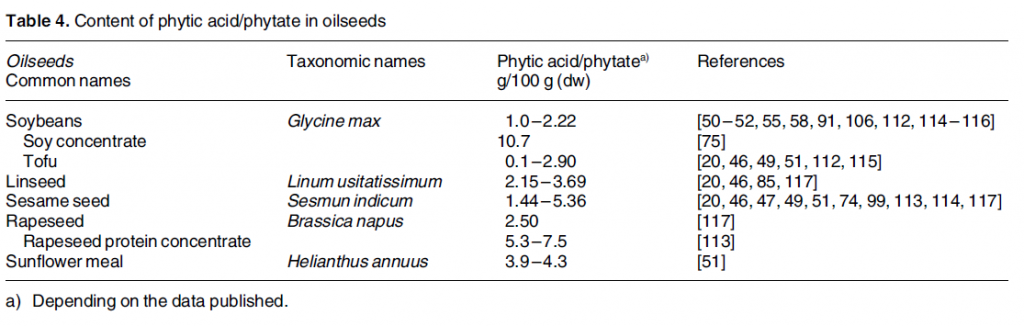
Phytic acid is phosphorus stores in nuts, edible seeds, beans/legumes, and grains. It is often referred to as anti-nutrient. Phytates (phytic acid) have been shown to decrease absorption of minerals, including iron, calcium, zinc and manganese. Phytates decrease the absorption by binding to the minerals before their uptake in the stomach and intestines. 5-10mg of phytic acid can decrease iron absorption by 50%. 1 This research done on non-WLS patients but is something to be aware of if you are having iron deficiency anemia or low calcium issues.
There are ways to combat the effects of phytic acid such as heat, soaking, fermenting, Vitamin C, protein, probiotics, and sprouting. 2
Phytic acid has many benefits such as preventing kidney stones, anti cancer effects, cardiovascular health protectant, binding with heavy metals and free radicals. It becomes an antioxidant and is a secondary messenger in cellular activity.
Phytate intake is something to be looked at if you are experiencing iron or calcium deficiencies.Adjusting your intake of phytates containing foods, combining them with high Vitamin C containing food items, and/or prepping them before consumption can decrease the mineral binding capacity. It would also be prudent to be aware of the timing between eating phytic acid containing foods and any vitamin or mineral supplementation.
Revision of Gastric Bypass
July 20, 2009 10:02 pm
Terry had the gastric bypass operation 3 years ago in an a major referral center by an established surgeon. The surgery went well, and lasted about one hour. The postoperative course was uneventful, and the patient was discharged home on post op day 2. The 3-6 month post-op period was complicated by a stricture at the gastro-jejunostomy anastomosis. An upper endoscopy and dilation. He continued to loose weight as expected. He attended the support meetings early on and then ended up missing some of them after the third year. The follow up appointments with the surgeon were all kept. The episodes of dumping syndrome, the feeling of passing out, diarrhea, high heart rate, nausea amongst others were scary early on. They became less frequent but not any less concerning. He was told by the surgeon that it s a part of the gastric bypass operation. In fact someone at the surgeons office told him that “..you hope you have it, since it will help you with your diet and prevent weight regain..”
He started feeling weak and tired at times after the second year. He also gained about 50 pounds back after the third year. The weight gain did not stop till I was within reach of my pre gastric bypass operation. What is worse is that he had to use CPAP machine for sleep apnea that had gone away with weight loss. He also was started back on some of his medications including those for diabetes. He went back to his surgeon, whose first reaction was that “….You must be doing something wrong…”
He was then referred to see the nutritionist, had an upper endoscopy, and an upper GI series. When he went back, he was told that there is nothing wrong and that he should eat correctly and exercise more.
This is not a story but a real example of many more patient that I see in our office all the time. As the facts are pretty accurate, clearly the name, and the specific details have been altered in this article.
What this patient has experienced is what I hear in the office all the time from patients who had the gastric bypass and they “….did not know….” about any other weight loss surgical procedure. After the surgical “honey moon” period of about 2-3 years (much longer than my real honey moon) the reality sets in. Weight regain, inadequate weight loss, nutritional deficiencies, dumping syndrome, and solid intolerance are examples of problems which will direct a patient to seek a solution.
The published data show that the small size of the pouch, in gastric bypass, does not predict excess weight loss (O’Connor et.al. SOARD 4, 2008, 399-403), (Nishie et.al, Obesity Surgery 17, 2007, 1183-1188). The size of the gastrojejunostomy anastomosis also does not assure adequate weight loss (Cottam et.al. Obesity Surgery 19, 2009, 13-17). Dumping syndrome does not improve gastric bypass surgery outcome. And the incidence of resolution of the obesity related illnesses is significantly better with duodenal switch operation that the gastric bypass or the adjustable gastric banding procedure. Patients with diabetes or cholesterol and triglyceride problem, in my opinion, should not have gastric bypass or adjustable gastric banding done.
A review of the published scientific articles in JAMA, shows that the outcome of Duodenal switch operation is far better than the alternatives with all measured parameters of excess weight loss, diabetes resolution, and improvement of hyperlipidemia.
Let me pose a question. If a patient is told that there are two antibiotics and one of them will treat the urinary track infection in 83.7% of the time and the alternative will treat it in 98.9% of the time, which one would you like to be treated with, if the overall risks all the same?
| Significant Hyperlipidemia Improvement | Diabetes Resolution |
Excess Weight Loss |
|
| Duodenal Switch | 99.50% | 98.90% | 70.10% |
| Gastric Bypass | 93.60% | 83.70% | 61.60% |
| Gastroplasty | 80.90% | 71.60% | 68.20% |
| Gastric Banding | 71.10% | 47.90% | 47.50% |
Source:JAMA, review of published data based on more than 22000 patients outcome.
As a Duodenal switch surgeon the answer is clear. I am only trying assure that no patient ever goes to the operating room without having all their options entertained. An informed consent is only valid if all the information was presented. Too often the alternative are either never discussed or barely discussed. A review of the websites demonstrates this point. Very few surgical practices that do not offer the duodenal switch operation discuss this alternative.
And to those that ask, “Why are there more surgeons doing the duodenal switch operation?” I think this a question that needs to be posed to those that do not do it. Here are some of the reasons:
- The perceived malnutrition is usually given as a reason. There is a large body of published data in the literature that documents the incidence of malnutrition to be significant in gastric bypass operation. In fact, because of the dietary restriction after gastric bypass there are as many if not more nutritional deficiencies that develop after this operation than the duodenal switch operation.
- The need for follow up. I am not clear as to why would this be a reason not to offer a surgery. The scientific evidence again shows that the more structured the follow up the better the outcome. Obesity is a chronic disease, that has a surgical, medical and maintenance phase. The broad picture of treatment plan for obesity in my opinion is no different than that of a cancer patient, who may need surgery, followed by chemo-radiation, and routine follow up.
- Last, and most vividly discussed is the issue of increased flatus, and loose bowel movements. There is no dispute that the duodenal switch operation does cause increase in flatulence and loose bowel movement. But here are the facts- in my more than 10 years in private practice, in an office that at times the waiting room is full of pre and post op patients, we have never had to evacuate the building because someone let one go! It has been my experience that that in overwhelming number of cases that have problem with significant gas and diarrhea the problem is easily corrected with minor changes in diet. Polish sausage, bagel and cream cheese for breakfast, deep dish pizza for lunch, and deep fried turkey may give some patients increased gas and diarrhea! With this said however, I have had patients in whom after exhausting all non surgical options (dietary modifications, medications etc) revision of the duodenal switch operation has been done.
In my opinion, the best patient is the most knowledgeable patient. Please make sure that you have taken the time to investigate not only the the surgeon, but also the available procedures.

