Weight loss Medications compared to surgery
February 20, 2024 5:44 pm
SIPS-SADI and ASMBS
December 31, 2023 1:21 pm
Survey
December 16, 2023 9:54 am
Long Term Outcome SurveyExclusive Member Content
December 01, 2023 9:08 am
Weight Loss Injection
May 10, 2023 1:06 pm
Semaglutide (Ozempic, Rybelsus, Wegovy, Saxenda) and tripeptide (Mounjaro) treat type II diabetes. They work thru several complex pathways. An observed side effect that has been noted in diabetic patients has been weight loss.
Some have been advocating using the class of medications for weight loss. However, Wegovy is the only medication approved for weight loss in non-diabetic patients.
There is a lot to be discussed here:
1-the use of the medications for weight loss is an off-label use (except Wegovy)- meaning that the FDA did not approve the medication as a weight loss drug.
The practical implication is that the medication’s safety and complication profile in non-diabetic patients looking to lose weight may be unknown and has not been studied.
2-The medication has become available thru compounding pharmacies. It is crucial to appreciate that compounding medications do not meet the same rigor and standards and may, in fact, not be the same formula as the FDA has stated.. This also means that a compounding pharmacy does not approve the medications in several states.
3-The most critical issue for me is the lack of a “long-term plan.” It is not clear what would happen when the patient stopped the medication. Will the patient experience weight regain? Will the patient require higher doses of the medication to maintain the weight loss, or will the medication stop working altogether? Unfortunately, we do not have these answers. For those skeptical about my questions, let me remind you that phentermine has significant side effects, and almost all patients experience weight gain when they have to stop the medication because of the cardiovascular complication of medication.
Pictures For Anesthesia
February 02, 2022 11:57 am


Bariatric Surgery 2022
January 23, 2022 10:57 pm
The PowerPoint presentation: Meeting-Jan 22
The PDF presentation: Meeting-Jan 22
References : https://www.dssurgery.com/articles/bariatric-2022/
Elective Surgery and Anesthesia for Patients after COVID-19 Infection
January 23, 2022 6:03 pm


ASA and APSF Joint Statement on Elective Surgery and Anesthesia for Patients after COVID-19 Infection is also available for download (PDF)
Since hospitals are able to continue to perform elective surgeries while the COVID-19 pandemic continues, determining the optimal timing of procedures for patients who have recovered from COVID-19 infection and the appropriate level of preoperative evaluation are challenging given the current lack of evidence or precedent. The following guidance is intended to aid hospitals, surgeons, anesthesiologists, and proceduralists in evaluating and scheduling these patients. It is subject to change as new evidence emerges.
In general, all non-urgent procedures should be delayed until the patient has met criteria for discontinuing isolation and COVID-19 transmission precautions and has entered the recovery phase. Elective surgeries should be performed for patients who have recovered from COVID-19 infection only when the anesthesiologist and surgeon or proceduralist agree jointly to proceed.
What determines when a patient confirmed to have COVID-19 is no longer infectious?
The Centers for Disease Control and Prevention (CDC) provides guidance for physicians to decide when transmission-based precautions (e.g., isolation, use of personal protective equipment and engineering controls) may be discontinued for hospitalized patients or home isolation may be discontinued for outpatients.
Patients infected with SARS-CoV-2, as confirmed by reverse transcriptase-polymerase chain reaction (RT-PCR) testing of respiratory secretions, may be asymptomatic or symptomatic. Symptomatic patients may be further sub-classified into two groups depending upon symptom severity. Table 1 provides definitions of these COVID-related illness levels of severity.
- Patients with mild to moderate symptoms* (generally those without viral pneumonia or oxygen saturation below 94 percent)
- Patients who experienced severe or critical illness** due to COVID-19 (e.g., pneumonia, hypoxemic respiratory failure, septic shock).
Severely immunocompromised patients***, whether suffering from asymptomatic or symptomatic COVID-19, are considered separately.
Current data indicate that, in patients with mild to moderate COVID-19, repeat RT-PCR testing may detect SARS-CoV-2 RNA for a prolonged period after symptoms first appear. However, in these patients, replication-competent virus has not been recovered after 10 days have elapsed following symptom onset. Considering this information, the CDC recommends that physicians use a time- and symptom-based strategy to decide when patients with COVID-19 are no longer infectious.
For patients with confirmed COVID-19 infection who are not severely immunocompromised and experience mild to moderate symptoms*, the CDC recommends discontinuing isolation and other transmission-based precautions when:
- At least 10 days have passed since symptoms first appeared.
- At least 24 hours have passed since last fever without the use of fever-reducing medications.
- Symptoms (e.g., cough, shortness of breath) have improved.
For patients who are not severely immunocompromised and have been asymptomatic throughout their infection, isolation and other transmission-based precautions may be discontinued when at least 10 days have passed since the date of their first positive viral diagnostic test.
In approximately 95 percent of severely or critically ill patients (including some with severe immunocompromise), replication-competent virus was not present after 15 days following the onset of symptoms. Replication-competent virus was not detected in any severely or critically ill patient beyond 20 days after symptom onset.
Therefore, in patients with severe to critical illness** or who are severely immunocompromised***, the CDC recommends discontinuing isolation and other transmission-based precautions when:
- At least 10 days and up to 20 days have passed since symptoms first appeared.
- At least 24 hours have passed since the last fever without the use of fever-reducing medications.
- Symptoms (e.g., cough, shortness of breath) have improved.
Consultation with infection control experts is strongly advised prior to discontinuing precautions for this group of patients. Clinical judgment ultimately prevails when deciding whether a patient remains infectious. Maintaining transmission-based precautions and repeat RT-PCR testing may be appropriate if clinical suspicion of ongoing infection exists. The utility of repeat RT-PCR testing after improvement in symptoms is unknown as patients will frequently remain at least intermittently positive for weeks to months.
If a patient suspected of having SARS-CoV-2 infection is never tested, the decision to discontinue transmission-based precautions can be made using the symptom-based strategy described above.
Other factors, such as advanced age, diabetes mellitus, or end-stage renal disease, may pose a much lower degree of immunocompromise; their effect upon the duration of infectivity for a given patient is not known.
Ultimately, the degree of immunocompromise for the patient is determined by the treating provider, and preventive actions are tailored to each individual and situation.
What is the appropriate length of time between recovery from COVID-19 and surgery with respect to minimizing postoperative complications?
The preoperative evaluation of a surgical patient who is recovering from COVID-19 involves optimization of the patient’s medical conditions and physiologic status. Since COVID-19 can impact virtually all major organ systems, the timing of surgery after a COVID-19 diagnosis is important when considering the risk of postoperative complications.
There are limited data now that address timing of surgery after COVID-19 infection. One study found a significantly higher risk of pulmonary complications within the first four weeks after diagnosis (1). An upper respiratory infection within the month preceding surgery has previously been found to be an independent risk factor for postoperative pulmonary complications (2). Patients with diabetes are more likely to have severe COVID-19 disease and are more likely to be hospitalized (3,4). Studies conducted during the 2009 influenza A H1N1 pandemic found that pulmonary function continues to recover up to three months after ARDS (5).
Given this current knowledge base, wait times before surgery can be reasonably extrapolated and are a suggested starting point in the preoperative evaluation of the COVID-19-recovered patient.
The timing of elective surgery after recovery from COVID-19 utilizes both symptom- and severity-based categories. Suggested wait times from the date of COVID-19 diagnosis to surgery are as follows:
- Four weeks for an asymptomatic patient or recovery from only mild, non-respiratory symptoms.
- Six weeks for a symptomatic patient (e.g., cough, dyspnea) who did not require hospitalization.
- Eight to 10 weeks for a symptomatic patient who is diabetic, immunocompromised, or hospitalized.
- Twelve weeks for a patient who was admitted to an intensive care unit due to COVID-19 infection.
These timelines should not be considered definitive; each patient’s preoperative risk assessment should be individualized, factoring in surgical intensity, patient co-morbidities, and the benefit/risk ratio of further delaying surgery.
Residual symptoms such as fatigue, shortness of breath, and chest pain are common in patients who have had COVID-19 (6,7). These symptoms can be present more than 60 days after diagnosis (7). In addition, COVID-19 may have long term deleterious effects on myocardial anatomy and function (8). A more thorough preoperative evaluation, scheduled further in advance of surgery with special attention given to the cardiopulmonary systems, should be considered in patients who have recovered from COVID-19 and especially those with residual symptoms.
Is repeat SARS-CoV-2 testing needed?
At present, the CDC does not recommend re-testing for COVID-19 within 90 days of symptom onset (9). Repeat PCR testing in asymptomatic patients is strongly discouraged since persistent or recurrent positive PCR tests are common after recovery. However, if a patient presents within 90 days and has recurrence of symptoms, re-testing and consultation with an infectious disease expert can be considered.
Once the 90-day recovery period has ended, the patient should undergo one pre-operative nasopharyngeal PCR test ideally ≤ three days prior to the procedure.
References
- COVIDSurg Collaborative. Delaying surgery for patients with a previous SARS‐CoV‐2 infection. BJS 2020; 107: e601–e602. https://doi.org/10.1002/bjs.12050
- Canet J, Gallart L, Gomar C, et al. Prediction of postoperative pulmonary complications in a population-based surgical cohort. Anesthesiology 2010;113:1338. https://doi.org/10.1097/ALN.0b013e3181fc6e0a
- Guan WJ, Liang WH, Zhao Y, et al. Comorbidity and its impact on 1590 patients with Covid-19 in China: a nationwide analysis. Eur Respir J 2020. DOI: 10.1183/13993003.00547-2020
- Petrilli CM, Jones SA, Yang J, et al. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study. BMJ 2020;369:m1966 doi: https://doi.org/10.1136/bmj.m1966.
- Hsieh M-J, Lee W-C, Cho H-Y, et al. Recovery of pulmonary functions, exercise capacity, and quality of life after pulmonary rehabilitation in survivors of ARDS due to severe influenza A (H1N1) pneumonitis. Influenza and other respiratory viruses. Apr 2018. https://doi.org/10.1111/irv.12566
- Tenforde MW, Kim SS, Lindsell CJ., et al. Symptom Duration and Risk Factors for Delayed Return to Usual Health Among Outpatients with COVID-19 in a Multistate Health Care Systems Network – United States, March-June 2020. MMWR 2020 Jul 31;69(30):993-998. https://dx.doi.org/10.15585%2Fmmwr.mm6930e1
- Carfi A, Bernabei R, Landi F., et al. Persistent Symptoms in Patients After Acute COVID-19. JAMA July 9, 2020. doi:10.1001/jama.2020.12603
- Puntmann VO, Carerj ML, Wieters I, et al. Outcomes of Cardiovascular Magnetic Resonance Imaging in Patients Recently Recovered From Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 2020;5(11):1265-1273. doi:10.1001/jamacardio.2020.3557
- https://www.cdc.gov/coronavirus/2019-ncov/hcp/duration-isolation.html
Accessed Oct 28, 2020
Table 1: Definitions for Severity Levels of COVID-Related Illness
The studies used to inform the guidance in this joint statement do not clearly define “severe” or “critical” illness. The definitions in the National Institutes of Health (NIH) COVID-19 Treatment Guidelines (cited under references below) are suggested to categorize disease. The highest level of illness severity experienced by the patient at any point in their clinical course should be used.
* Mild Illness: Signs and symptoms of COVID-19 (e.g., fever, cough, sore throat, malaise, headache, muscle pain) without shortness of breath, dyspnea, or abnormal chest imaging.
* Moderate Illness: Evidence of lower respiratory disease by clinical assessment or imaging and oxygen saturation (SpO2) ≥94 percent on room air at sea level.
** Severe Illness: Respiratory rate >30 breaths per minute, SpO2 <94 percent on room air at sea level (or, for patients with chronic hypoxemia, a decrease from baseline of >3 percent), a ratio of arterial partial pressure of oxygen to fractional inspired oxygen (PaO2/FiO2) <300 mmHg, or lung infiltrates involving >50 percent of the lung fields.
** Critical Illness: The presence of respiratory failure, septic shock, and/or multiple organ dysfunction.
*** The studies used to inform this guidance did not clearly define “severely immunocompromised.” For the purposes of this guidance, “severely immunocompromised” refers to patients:
-
- Currently undergoing chemotherapy for cancer.
- Within 1 year of receiving a hematopoietic stem cell or solid organ transplant.
- Having untreated HIV with a CD4 T lymphocyte count <200.
- Having a combined primary immunodeficiency disorder.
- Treated with prednisone >20mg/day for more than 14 days.
Reference sources from CDC and NIH websites as of 22 Sept 2020:
Interim Clinical Guidance for Management of Patients with Confirmed Coronavirus Disease (COVID-19)
https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-guidance-management-patients.html
Overview of testing
https://www.cdc.gov/coronavirus/2019-ncov/hcp/testing-overview.html
Discontinuation of Transmission-Based Precautions and Disposition of Patients with COVID-19 in Healthcare Settings (Interim Guidance)
https://www.cdc.gov/coronavirus/2019-ncov/hcp/disposition-hospitalized-patients.html
Duration of Isolation and Precautions for Adults with COVID-19
https://www.cdc.gov/coronavirus/2019-ncov/hcp/duration-isolation.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fcommunity%2Fstrategy-discontinue-isolation.html
National Institutes of Health (NIH) COVID-19 Treatment Guidelines
https://www.covid19treatmentguidelines.nih.gov/whats-new/
A GUIDE TO COVID-19 TESTS FOR THE PUBLIC
January 23, 2022 5:38 pm
THE MAIN TESTS AVAILABLE FOR COVID-19
VIRUS STRUCTURE
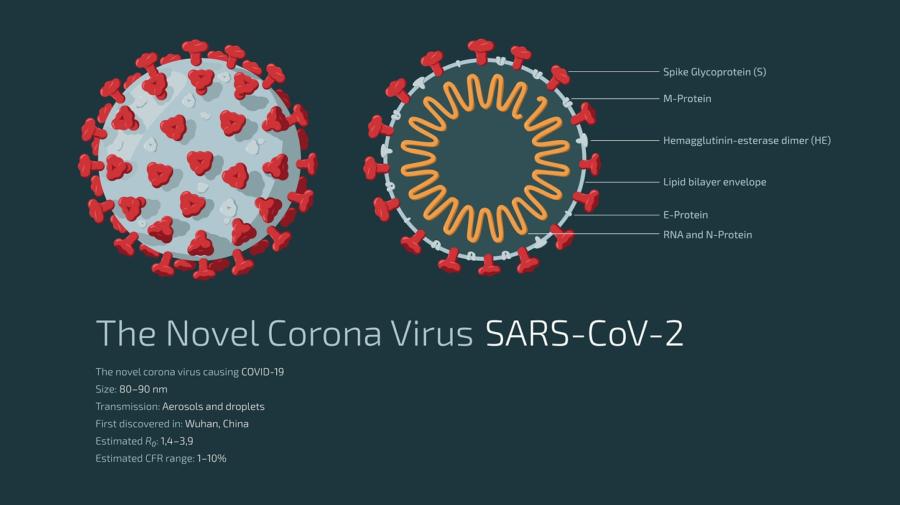 To understand testing methods, it is helpful to understand the structure of the coronavirus SARS-CoV-2, which causes the disease COVID-19.
The virus is composed of a core made up of nucleic acid (nucleic acids are what makes up the virus’s genetic code) in the form of RNA, surrounded by a coat called the envelope which contains various proteins. Spikes formed of a protein called the S (spike) protrude from the envelope. It is the S protein that attaches to cells of the human respiratory tract.
To understand testing methods, it is helpful to understand the structure of the coronavirus SARS-CoV-2, which causes the disease COVID-19.
The virus is composed of a core made up of nucleic acid (nucleic acids are what makes up the virus’s genetic code) in the form of RNA, surrounded by a coat called the envelope which contains various proteins. Spikes formed of a protein called the S (spike) protrude from the envelope. It is the S protein that attaches to cells of the human respiratory tract.
TESTING
The tests commonly available for SARS-CoV-2 can detect either:- the RNA − detected by the PCR test
- the surrounding proteins − detected by the rapid lateral flow devices
- the human body’s response to the virus – detected by antibody tests.
PCR TESTINGNUCLEIC ACIDS ARE WHAT MAKES UP THE VIRUS’S GENETIC CODE
PCR tests detect the virus’ RNA. These tests are normally carried out in a laboratory using a swab of the nose and/or throat. PCR tests can detect very tiny amounts of RNA, meaning they are extremely sensitive. They are the best test for current infection. Patients with COVID-19 usually start to become positive by PCR testing a day or two before symptoms start and will continue to test positive by PCR afterwards for some time. Repeat PCR once a diagnosis has been made is not necessary. The period the patient must isolate for is defined by time from the start of symptoms or, if there are no symptoms, from the first positive test. Current UK policy is that patients must self-isolate for ten days after this time.WHEN SHOULD I HAVE A PCR TEST?
- If you currently have symptoms that may indicate COVID-19, this is the test you should have to diagnose the infection.
- If a lateral flow test is positive. The purpose of the PCR test is to confirm the diagnosis, since it is a more accurate test than the lateral flow test.
IS A PCR TEST ACCURATE?
PCR is the most accurate test available for current infection. In a person with symptoms, a positive PCR test is likely to accurately indicate infection. If a person has symptoms suggesting infection but a negative PCR test, doctors may decide to repeat the test if they still suspect infection (e.g. in hospitalised patients).LATERAL FLOW TESTS
These are the rapid tests that are used in the community. They are convenient because they can give a result within 30 minutes and do not need a laboratory. They detect proteins from the virus, not RNA. They use a swab of the nose and/or throat and are carried out on a small flat plastic device like a pregnancy test. These tests are very different from PCR. They are not suitable for diagnosing individual patients who suspect they may be infected because they have symptoms. People with symptoms need a PCR test. Lateral flow tests are intended for picking up additional infected cases who would otherwise be missed because they don’t have any symptoms.WHEN SHOULD I HAVE A LATERAL FLOW TEST?
- You should only have this test if you don’t have any symptoms and have been invited to take one as part of an exercise to identify infected people without symptoms.
ARE LATERAL FLOW TESTS ACCURATE?
These tests are not as sensitive as PCR. They are simply a convenient way of picking up a proportion of undiagnosed people who have no symptoms. The way to look at these tests is that every additional positive case picked up is a bonus, preventing further unknown transmission of the virus. If a person tests positive with these tests, they need to confirm this by having a more accurate PCR. In the meantime, they must self-isolate. If these tests are negative, the person may or may not be infected and that person must continue to take the usual precautions such as hand washing, wearing a mask and social distancing. A negative lateral flow test should not be used to rule out infection or indicate that it is safe to do something such as visit relatives. You can read more about the accuracy of lateral flow tests here.ANTIBODY TESTS
These tests detect the body’s response to a previous infection, by looking for antibodies that the body has produced. It takes some time after infection for the body to produce antibodies. So, antibody tests are not suitable for diagnosing people at the time they have symptoms. They are useful for finding out if someone has been infected in the past. This is useful, for example, for studying how many people in a population have been infected. It is not known for how long after infection antibody tests remain positive. Levels of antibody are likely to decline with time, over months or years.WHEN SHOULD I HAVE AN ANTIBODY TEST?
- You might be asked to have an antibody test as part of a study to see how many people have been infected in the past.
- In future, if a doctor wanted to know if you had been infected in the past, they might perform an antibody test.
LAMP AND LAMPORE TESTING
Like RT-PCR, LAMP and LampORE tests detect the viral RNA. They have the advantage of being able to use saliva as a sample, as well as swabs. Recently LamPORE has been deployed for local community testing in some locations. This test can be carried out in mobile laboratories around the country. LamPORE tests have high accuracy. They can be used for people with or without symptoms, but they are currently being deployed in the UK to detect people without symptoms in the community. As these tests are more accurate than lateral flow tests, positive tests do not require a confirmation by PCR. Copied: Source https://www.rcpath.org/profession/coronavirus-resource-hub/guide-to-covid-19-tests-for-members-of-the-public.htmlCovid 19 Response
January 19, 2022 9:17 am

