Category: Duodenal Switch
Patch or Spray Vitamins
August 15, 2014 10:37 pm
At the last group meeting, there were several questions whether vitamin D and other vitamins would be absorbed via patch (transdermal) and spray (buccal/sublingual) routes. After reviewing several resources, the only article I could find was for transdermal Vitamin D absorption. However, if we look at the mechanism for each route we can make an educated assumption.
Transdermal route of absorption (without additional absorption enhancers) (ref) requires a molecular mass less than 500 g/mole, high lipophilicity (affinity to fat or lipids), and low required daily dose (less than 2mg). The fat-soluble vitamins are definitely lipophilic, all of them have molecular weights less than 500 g/mole and daily dose is under 2mg. It seems that hydrophilic medications (that have an affinity to water) may have less ability to be absorbed with this route unless a chemical enhancer is added to the product. Most vitamins and minerals have lower molecular weights except Vitamin B12 which has too high of a molecular weight unless an enhancer is added. The transdermal route has slower absorption than buccal (oral mucosa) but faster than usual tablet oral route. The down side to transdermal route is possible skin issues due to medication, adhesives, and also different rates of absorption due to skin thickness and condition.
Buccal/sublingual route of absorption is dependent on lipid solubility, oil to water partition coeffincient, saliva pH, small to moderate molecular weight, and oral mucosa thickness. The mechanism of action is osmosis, which means items that readily dissolve in water are easily absorbed. Unlike orally ingested medicates, that take time to absorb and need to be filtered and/or processed in the liver, sublingual route is fast absorbing and the liver is bypassed. The down side to this route is it disrupts eating and drinking and is not efficient with smoking due to vasoconstriction.
An e-mail was sent to the companies inquiring about the outcomes of their products with people with malabsorption issues. No response was received from the spray vitamin companies.A request was also sent to obtain any research articles they may have but a response has not been received at this time. The following is the response I received from the maker of Patch MD.
“I am the president and founder of Patch MD. We design Patch MD to help people that have digestive issues and malabsorption. Our whole premise is to avoid the digestive track, by doing so we avoid dealing with conditions such as short bowel syndrome, acid reflux, and bariatric surgery to name a few. People also with Crohn’s disease and iliac disease are challenged with digestion and absorption every day of their life. Our patches are designed specifically to pass nutrition through the skin into the bloodstream. We get letters every day from people that have had bariatric surgery and were unable to get vitamin D, calcium, the B’s and Vitamin A and K, our product works because we use the skin as our delivery system, absorption is through the skin, avoiding all digestive potential issues. The only problem that we may have is we tell our customers to use no lotions or cream in the patch application area, as you may understand it will prevent absorption. We are going to be at a national convention this weekend in Manhattan Beach California to take part and display our products at the ObesityHelp conference. They ask us to take part as they were getting great reviews from their members that are using the patch. All were improving their blood work after taking Patch MD patches.”
Earl Hailey, President Patch MD
In light of the review of data, it would seem that the transdermal route would be beneficial to people who are having issues maintaining blood levels of fat-soluble vitamin levels. The other vitamins also have a good prospect of absorption via transdermal route. Buccal or sublingual (sprays) would seem to have a better outcome for water-soluble vitamins unless there is an additive added to the product to increase the solubility of the fat-soluble vitamins and make them water miscible. We must realize that there is no data for Duodenal Switch patients and very little data regarding these routes of absorption with vitamins specifically. If you are going to try these types of vitamins you should be extremely diligent in following your laboratory studies for vitamin levels with greater frequency until it is determined they are maintaining your blood levels.
Also, it should be noted that water miscible (dry) Vitamin A, D, E, K are the only type of these vitamins a DS patients should be taking. Over the counter Vitamin A, D, E, K are fat-soluble and due to the fat malabsorption after DS these type of vitamins are not appropriate to maintain blood levels. Water miscible (dry) vitamins should NOT be taken with fatty or oily foods and should also be taken 30 minutes prior or 30 minutes after eating. The water miscibility makes them water soluble and therefore will not have optimal absorption if taken with fat. Fat also increases the rate of digestion through the small bowel after DS and decreases the amount of time the vitamin has in the bowel and therefore, decreases absorption. They are best absorbed when taken on their own.
The good news patches and spray routes of administering medications and supplements is an up and coming area of research. There are several ongoing research studies and new developments on the horizon for increasing absorbability of transdermal route with different types of additives and techniques.
August 6, 2014 Group Meeting Recap
August 08, 2014 6:35 pm
August’s group meeting/webinar topic was Vitamin D. Dr. Keshishian will be adding the voice over to the slides and it will be uploaded to when it’s completed. But in the meantime here are some highlights. Webinar here.
Vitamin D is a fat soluble vitamin has many important functions including bone health, cardiovascular health, blood glucose regulation, anti-cancer, anti-inflammatory, muscle function, respirator function, brain development and health, and immune function. There are several very large studies investigating other functions of Vitamin D. Vitamin D knowledge is in the midst of huge changes due to these upcoming studies.
Vitamin D metabolism is a complicated process whether via photo conversion in the skin or supplementation. Either way Vitamin D metabolism requires cholesterol to be converted to its active form. The fat-solubility is the primary reason for deficiency after Doudenal Switch, due to malabsorption of fat needed for conversion of Vitamin D. The Parathyroid gland helps to regulate absorption of Vitamin D. It is an inverse mechanism, meaning a high Parathyroid level signals more absorption of Vitamin D and calcium also.
Vitamin D deficiency is a World Health Organization priority. There are several causes some related to sunscreen use, disease processes, WLS, cola intake, diet related and medications. These can compound Vitamin D deficiencies.
Dr. Keshishian has new guide lines for Vitamin D levels. Due to the changing research regarding Vitamin D these guidelines are changing. There are some endocrinologists in Vitamin D research that are recommending even high standard of Vitamin D. DS patients should be well above the border of insufficient and sufficient due to underlining contributing facts for deficiencies and the lack of absorption. Parathyroid Hormone levels are inversely related. High PTH level can indicate Vitamin D deficiency and increase need for calcium. Calcium blood levels are not a good indicator of calcium or Vitamin D needs as the body is efficient at maintaining Calcium blood levels by breaking down bone mass due to the critic bodies need for circulating calcium.
Supplementation options are as follows: Please note that most over the counter Vitamin D is not appropriate for DS absorption. DS patients need to take “Dry” water miscible Vitamin D3. Please see the previous blog post regarding https://blog.dssurgery.com/2013/08/vitamin-d-and-dry-water-soluble.html for more information and pictures of this type of Vitamin D. Vitamin D is tied to several other nutrients for metabolism such as protein, calcium, magnesium, zinc and potassium. Treatment for correcting iron deficiency and phosphorus intake counter act Vitamin D absorption as do other previous discussed dietary issues. Take oral Vitamin D supplements even if you are receiving injectable Vitamin D.
Be proactive in Vitamin D supplements by monitoring your yearly DS laboratory studies. Please call the office with any questions. If in need of Vitamin D injections please see the previous blog post for related research article and compounding pharmacies. Vitamin D injections are not common place.
Please take the Vitamin D injections post to your treating physician if you are unable to see Dr. Keshishian and are in need of Vitamin D injections. If your treating physician has any questions please let them know Dr. Keshishian is available to answer their questions.
Our food selections for the meeting where all high Vitamin D recipes. Tuna stuff mushroom (Tuna for Vitamin D and mushrooms are a good source of zinc), crustless artichoke and spinach quiche ignore the part of the recipe for the crust and just bake in pie plate without the crust, Panna cotta with a strawberry balsamic compote and toasted flax seed and hemp hulls. The panna cotta is made with milk or almond milk and gelatin which are all important in bone health. Hemp hulls are a protein source as is the milk.
Strawberry Balsamic Compote taken from https://nomnompaleo.com
1/4 C balsamic Vinegar
2C hulled strawberries, thinly sliced
2 TBSP honey
1 TBSP fresh lemon juice
1tsp vanilla extract
1/4 tsp salt
In a sauce pan heat Balsamic vinegar until reduced by half and is a thick syrup. Add the rest of ingredients and simmer over medium heat for 5-10 minutes. Remove pan from heat and use an immersion blender to puree some of the sauce. The texture is to your liking, so puree as much or as little as you would like. Store in a sealed container for up to a week or you can freeze it for long term storage. This site also has a almond milk Panna Cotta but this is not the recipe use at the group meeting.
Panna Cotta Recipe
1/2 C 2% milk mix with 2 1/2 tsp of unflavored gelatin in a bowl to rehydrate the gelatin let sit for 5-10 minutes
In a medium saucepan mix
3 C 2% milk or whole milk
one vanilla bean split in half or 1 tsp vanilla extract
2 TBSP maple syrup
1 tsp salt
heat until steaming but not boiling, about 5-7 minutes. Take off heat.
Mix 1/4C greek style yogurt into the milk and rehydrated gelatin. Then whisk about 1 C of hot milk mixture into the gelatin/milk. Add this mixture into pan of hot milk and whisk well. Pour hot Panna Cotta mixture into ramekins. Refrigerate until set, about 2 hours.
In a small frying pan toast 2 TBSP Flax seed and mix with 2 TBSP hemp hulls. Before serving top with Strawberry Balsamic Compote and flax seed/hemp seed mixture to your taste.
Protein Malnutrition Protein Part 2
July 31, 2014 1:25 pm
Protein energy malnutrition (PEM) or Protein Malnutrition is a problem that can effect a few after weight loss surgery (WLS) and Duodenal Switch (DS). In our previous blog post on protein we discussed the types of essential and non-essential Amino Acids and possible sources. We also discussed how to choose the best bioavailable protein and to vary protein sources to achieve adequate protein levels. There are cases even with adequate protein intake that can result in PEM due to inadequate protein absorption. The early signs of low protein may be low energy, muscle weakness, moodiness, inability to sleep well, joint pain, changes in hair and nails and carb craving. It is imperative after WLS that you maintain your protein levels throughout your lifetime. The minimum protein intake is 80-100 grams per day after WLS. There is no leeway where protein is concerned. It is important in almost ever function in the body.
There are two types of protein energy malnutrition, Kwashiorkor and Marasmus:
Kwashiorkor is a lack of protein intake with adequate or slightly lower caloric intake. It’s symptoms are edema (swelling in legs, ankles, feet) enlarged abdomen, irritability, anorexia, hair discoloration and loss, muscle weakness, changes in psychomotor function, mental lethargy, ulcerations, brittle nails, rash or discoloration of the skin, bradycardia (slow heart rate), non-tender parotid enlargement, enlarged liver with fatty infiltrates that are similar to alcohol liver disease. The edema is caused by osmotic imbalance in the intestinal system causing swelling of the gut. Protein, primarily albumin is responsible for the colloidal pressure within the circulatory and tissue systems. The lack of protein within the circulatory systems cause fluids to “leak” into tissues causing edema. Gastro-intestinal symptoms can include nausea, vomiting, dehydration, diarrhea and increases in appetite. People who have pathological bacteria or parasites and/or after WLS diarrhea can precipitate lower levels of protein. If left untreated can lead to protein malnutrition.
Marasmus is characterized by a lack of protein and caloric intake. The symptoms are an emaciated appearance with edema. There is no liver changes as in Kwashiorkor. This is a starvation mode and can be difficult to treat and can progress to a point of no return.
Catabolysis is the bodies response to lack of protein and or nutrition. This biologic process breaks down muscle and fat to maintain bodily functions. Catabolysis is the body’s last resort to keep it alive. It is a starving body eating itself to keep vital organs alive.
Laboratory Studies are needed to determine the level of malnutrition and treatment routes. These studies include:
- Lipids
- CBC (complete blood count)
- CMP (comprehensive metabolic panel) includes liver and kidney function tests, Calcium and electrolytes
- Albumin Normal is greater than 3.5 gdL (transports nutrients such as calcium, zinc and Vitamin B6)
- Prealbumin (transthyretin) transports retinol (Vitamin A)
- Total protein Normal is greater than 6.3 gdL
- Iron tests such as serum iron, TIBC, and ferritin
- Vitamins and trace minerals such as B12 and folate, vitamin A, vitamin D, vitamin K, B vitamins, calcium, and magnesium
- Ova and Parasite stool testing
Protein is an extremely important nutrient within our bodies and is considered the workhorse in cells and organs. They are responsible for catalysts, messenger duties, structural, immunoprotectors, transporters, buffers, fluid balancers and many other roles. Protein has a hand in synthesizing other proteins, regulates protein turnover, enzyme activity, neurotransmission, gene transcription, transport of other nutrients, messenger and signals for growth hormone and insulin, structure, storage for other nutrients and immunity.
The muscular system is the most obvious structural protein in our bodies, 40% of the total body protein, as is hair, fingernails and cells. Our organs also require protein in order to function appropriately. However, protein’s role in red blood cell formation, size and health is extremely important. If you don’t have adequate protein levels your body can not make red blood cells. Transferrin is a protein that carries iron to receptors. Ferritin is an intercellular protein that stores iron until it is needed. Glycine is a protein for heme synthesis. B12 is also transported via a protein for red blood cell production. Protein is also important in blood clotting and plasma.
Cardiovascular health is also reliant on protein for structure and function. Also, proteins can have a protective effect at the mitochondrial level.
Kidney function relies on protein to regulate the acid base balance and ammonia disposal. The kidneys are also the site of amino acid production.
Protein is also important in bone health as a carrier for Vitamin K and calcium binding, tissue repair, healing and growth. Proteoglycans play a role in extracellular structures such as skin, bone, and cartilage. Also related to the skeletal system are glycoproteins, which also aid in building connective tissue, collagen, elastin and bone matrix.
Central Nervous system relies on proteins for neurotransmission, hormone production and other functions. Protein deficients can lead to neurologic problems such as altered behavior and mental function among other manifestations. The neuorpeptides have actions on transmission functions, mood and behavior. They can also effect a wide range of functions such as blood pressure, body temperature, pain sensation, and learning ability.
Immonoproteins are the group of proteins that provide immune protection such as immunoglobulins and antibodies.
Protein also have storage roles for copper, iron and zinc called metalloproteins. Copper and zinc are considered neurotransmitters, important for iron metabolism, and connective tissue formation in heart, blood vessels and skeletal.
There are situation where your protein needs will increase. In cases of wounds, burns, surgery, stress, sepsis or other illnesses, protein requirements increase. Also age, pregnancy, lactating and increased exercise increases protein needs.
Protein Energy Malnutrition is protein deficit that can and should be avoided after WLS. PEM, if left untreated, can lead to organ failure and death. Protein is crucial in almost every function of the body and without adequate levels there will be symptoms and side effects. Please take care to maintain your protein levels throughout your life. We have discussed several of protein’s function, however, there are many more.
Probiotics, C. diff & Enteric HyperoxaluriaExclusive Member Content
July 26, 2014 3:21 pm
Injectable Vitamin D Information and Research Articles
July 11, 2014 1:06 am
Injectable Vitamin D may be needed in some cases of Vitamin D deficiency or inability to increase Vitamin D level with oral supplements. Vitamin D is a fat soluble vitamin. It plays an important role in bone metabolism and structure. It has also been found to affect the immune regulation, control off- inflammatory reactions, and also be involved in a number of broad cellular functions throughout the body. Until a few years ago, very little attention was given to vitamin D levels. More recently, we have realized that due to a number of factors, there is a tendency for vitamin D deficiency to be present in the U.S. adult population. This finding is even more pronounced and severe in overweight patients.
The recommended dose for vitamin D supplements is much larger today than it was a few years ago. For example, it is not too uncommon to recommend an average dose of a 50,000 (IU) international unit of vitamin D by mouth on a daily basis after the duodenal switch operation.
Since vitamin D is a fat soluble vitamin, it is important that the appropriate type be utilized. Dry formulation of vitamin D is needed to ensure adequate absorption. There are a number of manufacturers that produce these. When searching for Dry Vitamin D the type a patient should be looking for is “Dry” D3-50. Some larger supplement manufacturer’s carry these products. The links to these manufacturers is located here. The “Dry” type of Vitamin D should NOT be taken with fatty or oily foods. Also to optimizes absorption they should be taken either 30 minutes prior to eating food or 30 minutes after eating.
If you are deficient in Vitamin D after trying “Dry” or water miscible Vitamin D then intramuscular Vitamin D injections might be an effective way to normalize your Vitamin D levels. Vitamin D can be formulated and purchased from any compounding pharmacies that are equipped and experienced in the interpretation of injectable vitamins and minerals. Your primary care WILL need to contact the compounding pharmacy of their choose for the recommendations and be willing to make the injections available to you. UNLESS you have been told to stop taking your daily “Dry” Vitamin D tablet supplement you should continue taking it after the injection.
We are supplying the following so that your PCP will understand the research behind injectable Vitamin D and to hopefully ensure that every patient is armed with this knowledge. Vitamin D deficiencies are becoming more common place in society due to the use of sunscreen and sun shielding clothing and hats, not only Duodenal Switch patients.
This is a research paper out of Finland that discusses injectable Vitamin D for the aged. The information can translate to anyone who finds themselves in a Vitamin D deficit state. https://www.gwern.net/docs/nootropics/1992-heikinheimo.pdf
This research paper is out of Australia where despite then sun drenched climate they are experiencing a large amount of people with Vitamin D deficiencies due to sunscreen, veiling, malabsorption, etc.
https://www.direct-ms.org/pdf/VitDGenScience/Vit%20D%20deficiency%20Australia%20art%20and%20ed.pdf
Below find the order sheet with the Injectable Vitamin D concentration listed. The common dosing for the vitamin D is 600,000 IU, deep IM every 6 months till the levels are normalized. The patient then can take the oral supplements only.
Finally, this is an except from an another Australian research paper describing the use of Megadoses of injectable Vitamin D in patients after Biliopancreatic Diversion which has a malabsorptive component similar to Duodenal Switch.
What size is my Bougie?
July 10, 2014 6:57 pm
A Bougie is a flexible plastic tube that comes in different sizes. It can be used to calibrate the size of the stomach during the duodenal switch or Sleeve gastrectomy. It is also used to dilate strictures of the esophagus or the stomach.
I am commonly asked what size is the bougie that I use. My usual answer is that it is equivalent to a 38 or so, and that the size does not matter.
Many surgeons do not use these types dilators, but rather alternative tubes that function as a sizer and a suction tube to eliminates the need for multiple tube insertions and removals.
The July 2014 publication of Obesity Surgery had and article by Spivak et.al. titled “Laparsocopic Sleeve Gastrectomy Using 42-French Versus 32-French Bougie: The First-Year Outcome.” In conclusion they reported that using 42 vs 32 French Bougie does not influence the weight loss of resolution of the combed condition in the first year.
There also other studies that support the position of erring on the side a larger sizer, a 40-French, to decrease the leak rate without having an impact on the excess weight loss at 3 years time.
The take home massage is that the size of the stomach after the sleeve does not predict the outcome of the weight loss surgery independently. There are multiple factors in play such as age, amount of excess weight, diet adherence and exercise.
July 2, 2014 Group Meeting Recap
July 03, 2014 7:11 am
First and foremost, We apologize for the confusion and last minute change with the webinar. It was set to go and logged in then the internet dropped the group meeting. The meeting site automatically marked the meeting as over. We sent out e-mails with the new URL for the group meeting but it took time. Thank you for your patience with this new platform. Although far reaching, it comes with downsides and hopefully we can make this a long term way to reach our patients. Lesson learned, don’t rely on wireless internet access for webinars. The Anemia slides will be added to our website dssurgery.com soon.
Ferritin is a protein that acts like your savings account. It’s like a holding tank. When you have a blood loss your body goes to Ferritin stores for iron to increase red blood cell production. Iron is like money in your pocket. For small and daily building of red blood cells. Transferrin is a protein transport that carries the iron. Copper is also needed to transport iron. Iron can be readily available but will not be utilized unless your protein levels are adequate. The protein level on laboratory studies needs to be at least 6 gm/dL & Albumin 3.2 gm/dL for adequate iron utilization. Vitamin B12 also is needed for iron utilization.
Iron metabolism in the DS patient is limited due to several factors. In unaltered anatomy Iron enters the stomach where it is exposed to acid and changes into a form which allows it to be absorbed. Then it enters the duodenum which is the chief area of the small intestines where iron absorption takes place. There is possibly a second minor site of absorption near the end of the ileum. However, after the DS there is a small portion of the duodenum that is left after the pyloric value for iron absorption. Below is a list of iron rich foods. Also remember to take Vitamin C with your iron supplements and when eating plant based iron rich foods add a food that is high in Vitamin C.
There was a brief discussion regarding Calcium oxalate kidney stones. That talk can be found on our website. Treatment is limiting oxalate containing foods and to increase calcium supplements to 3,000mg daily but to take half with food and the other half without food. Also Vitamin K2 can also decrease kidney stones.
Fissures where also briefly discussed. Fissures are most likely caused by the unopposed bile salts entering the colon after DS. Bile is alkaline and causes irritation to the mucosa. Treatment is liberal use of barrier type creams/ointments, controlling loose stools by watching if certain food items cause them or by using fiber with half the liquid mixed with it. The fiber with less liquid acts as a sponge to give more form to the stool.
We had anemia themed snacks at the live group meeting. Pate, Southwest ground Bison, and a Mayan Pumpkin seed dip. Here is the information on the nutritional value of Bison versus other meats. It is higher in iron and Vitamin B12 and lower in fat and cholesterol.
Iron Content of Common Foods
This chart shows the amount of total iron in food. Iron from most animal sources (heme iron) usually is more readily absorbed than iron from plant sources of food (non-heme iron). Include a source of vitamin C or heme iron to improve the absorption of non-heme iron.
Sources of Predominantly Heme Iron
|
FOOD
|
IRON (MILLIGRAMS)
|
|
Beef liver, braised (3 oz)
|
5.8
|
|
Lean sirloin, broiled (3 oz)
|
2.9
|
|
Lean ground beef, broiled (3 oz)
|
1.8
|
|
Skinless chicken breast, roasted dark meat (3 oz)
|
1.1
|
|
Skinless chicken breast, roasted white meat (3 oz)
|
0.9
|
|
Pork, lean, roasted (3 oz)
|
0.9
|
|
Salmon, canned with bone (3 oz)
|
0.7
|
Sources of Non-Heme Iron
|
FOOD
|
IRON (MILLIGRAMS)
|
|
Fortified breakfast cereal (1 cup)*
|
4.5 – 18
|
|
Pumpkin seeds (1 oz)
|
4.2
|
|
Blackstrap molasses (1 Tablespoon)
|
3.5
|
|
Soybean nuts (1/2 cup)
|
3.5
|
|
Bran (1/2 cup)
|
3.0
|
|
Spinach, boiled (1/2 cup)
|
3.2
|
|
Red kidney beans, cooked (1/2 cup)
|
2.6
|
|
Prune juice (3/4 cup)
|
2.3
|
|
Lima beans, cooked (1/2 cup)
|
2.2
|
|
Tofu, firm (1/2 cup)
|
2.0
|
|
Enriched rice, cooked (1/2 cup)
|
1.4
|
|
Pretzels (1 oz)
|
1.2
|
|
Whole-wheat bread (1 slice)
|
0.9
|
|
Green beans, cooked (1/2 cup)
|
0.8
|
|
White bread, made with enriched flour (1 slice)
|
0.8
|
|
Egg yolk, large (1)
|
0.6
|
|
Peanut butter, chunky (2 tablespoons)
|
0.6
|
|
Apricots, dried (3)
|
0.6
|
|
Zucchini, cooked (1/2 cup)
|
0.3
|
|
Cranberry juice (3/4 cup)
|
0.3
|
|
Unenriched rice, cooked (1/2 cup)
|
0.2
|
|
Grapes (1/3 cup)
|
0.1
|
|
Egg white, large (1)
|
From: The American Dietetic Association’s COMPLETE FOOD & NUTRITION GUIDE, 2nd ed. 2002.
USDA National Nutrient Database
Diabetes and Weight loss Surgery
June 30, 2014 5:44 pm
Diabetes should be considered as a family of diseases sharing a common name. They are different diseases because the cause, pathophysiology, and the treatment options are different for each diseases. This is not to say that there are not commonalities between them.
- Type I (Insulin deficiency, Juvenile onset)
- Type II (Insulin Resistance, Adult onset)
- Latent Autoimmune diabetes (LADA)
- Gestational
Type I diabetic patients requires insulin for control of their blood sugar. Insulin deficiency is the underlying problem with type I diabetes. The causes of type I diabetes are many and some are poorly understood. It is presumed that viral infections, genetics, infections, chronic pancreatitis and autoimmune conditions may all be potential causes of type I diabetes.
Type II diabetes is an insulin resistance state. This means that the patients’ body may be making adequate level of insulin however, for a number of reasons, the insulin is not able to normalize the blood sugars. Some Type II diabetic patients may also require insulin during advanced stages, but in most cases the initial treatment is oral medications.
| Diabetes Type | Blood Sugar | Blood Insulin |
| Type I | High | Low-absent |
| Type II | High | High(early disease state) |
The table above summarizes the laboratory findings in a patient who is diagnosed with diabetes. The measured insulin can be distinguished in the labs as being injected or patients own.
LADA is probably a subtype of Type I, with a delayed presentation. It behaves like Type I, with insulin deficiency, yet it is adult onset.
Gestational is more of a high blood glucose state during the pregnancy.
The goal of medical treatment for diabetes has been to normalize the blood sugars. There are no medical treatments regimens that correct any of the underlying causes of the Type I, or Type II.
In the case of Type I, the underlying case is Insulin deficiency. The definitive treatments may include Pancreatic transplantation, and intelligent Insulin pumps.
Surgical treatment of Type II, by some know and unknown mechanisms, corrects the underlying resistance to the insulin.
Weight loss surgical procedures have been shown to “cure” Type II”. The “remission” or “cure” rate of diabetes is really different between surgical procedures. Duodenal switch operation has been shown to have the highest remission-cure rate of all surgical procedures for the Type II diabetes. The references are available on our website. By definition, Type I can not be corrected-cured with weight loss surgery, since the underlying problem is insulin deficiency. What we have experienced however is that the Insulin requirements significantly decreases and blood glucose control is much easier after weight loss surgery.
There have been a number of articles reporting high relapse rate of Type II in gastric bypass patients. This is why I have always advocated that the patients with metabolic conditions, including diabetes should only consider the duodenal switch as their only surgical option.
The one study of 4434 patients, 68.2% of those patients who had Type II had remission within 5 years after the gastric bypass procedure. 35% of those patients, however, had a redevelopment of Type II after 5 years. “When the patients that never remitted and those that relapsed were added together, more than half of the patients (56%) did not have durable remission of diabetes.” (Obes Surg 2012 Nov 18:doi 10.1007/s11695-012-0802-1).
An article published in May 2010, reported 24% recurrence or worsening of the diabetes in patients who have had gastric bypass operation. (SOARD Volume 6, issue 3, May 201 249-253).
Single-Anastomosis DuodenoIleal Bypass (SADI)
June 23, 2014 6:30 pm
Single anastomosis duodenal switch, also known as Single Anastomosis DuodenoIleal Bypass (SADI) is a procedure that is being discussed in literature. There have been a few series of case reports that have been published in the last few years. I would like to review the procedure and share my opinion.
The theory behind the SADI has been to simplify the duodenal switch procedure. In “classical” duodenal switch procedure, the small bowel is divided in two places, (duodenum, and distal ileum) and two anastomosis are created (duodeno-ileostomy, and ileo-lieostomy). This can theoretically provide two potential places for leak, bleeding, adhesions as complications. In SADI, there is a single bowel division of the duodenum and a single anastimosis of the duodenum and the ileum. The sleeve component of the procedure is the same for both procedures. This is where their similarities end.
In the duodenal switch operation, the bowel is partitioned in to two parallel limbs- one that carries the biliopancreatic juices and a parallel limb that bring the food down from the post pyloric duodenum. They then join and form the common channel. The length of the biliopancreatic limb is so long that it does not allow bile to reflux back into the duodenum or back to the stomach causing the complication of bile reflux gastritis. With the single anastomosis of the SADI, the length of the bowel where the bile meets the duodenum is shorter than it is in normal anatomy. This significantly increases the possibility of the bile reflux. The second difference is the selective nature of the reduced absorption of the fat in the duodenal switch, in comparison to that of the carbohydrates. Duodenal switch operation has two absorptive lengths- the Alimentary channel, which is involved with protein and carbohydrate absorption, and the common channel that absorbs, fat, protein and carbohydrates. One can make changes to the common channel and impact the fat absorption significantly more than that of the carbohydrate and the proteins. In SADI procedure, that common channel and the alimentary limb are both the same- there is no way to selectively adjust the fat absorption without making significant changes to that of the protein and carbohydrate absorption.
There are a number of publications that have reported the short-term outcome of the SADI procedure. They appear promising, but they are short-term results. Long-term data is needed. If the outcome does not change significantly over time, then I could see a role for SADI in the treatment for obesity. In the mean time, patients need to be made aware that the suggestion that SADI is the same as the duodenal switch is probably not correct since we do not have the data to support this oversimplification.
Phytates the anti-nutrient?
June 20, 2014 3:33 pm
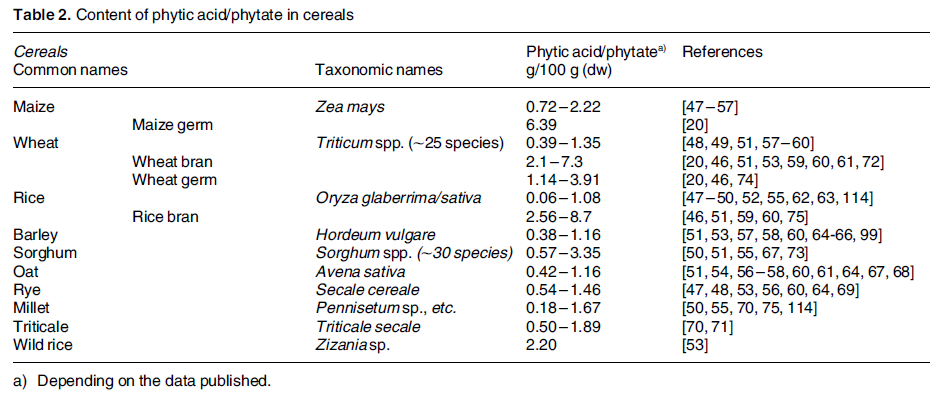
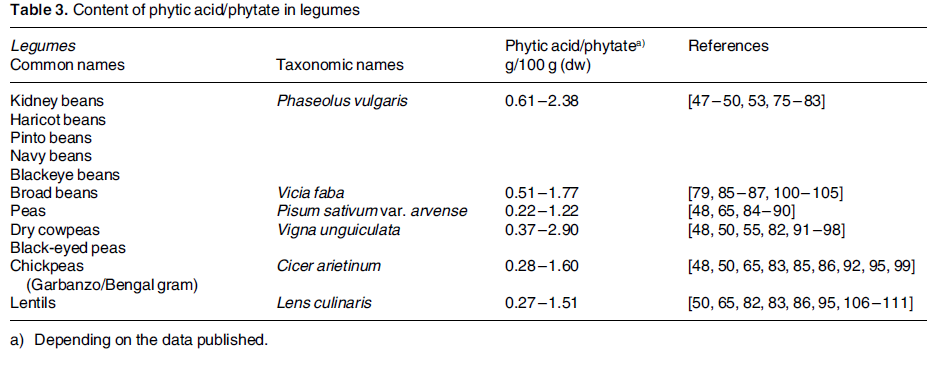
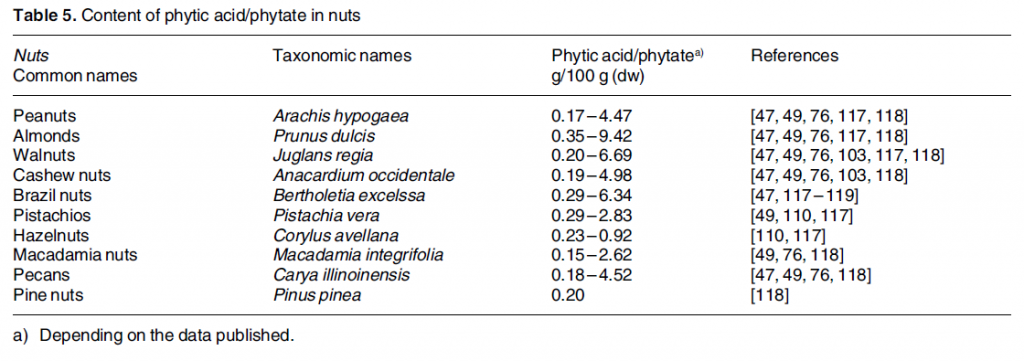
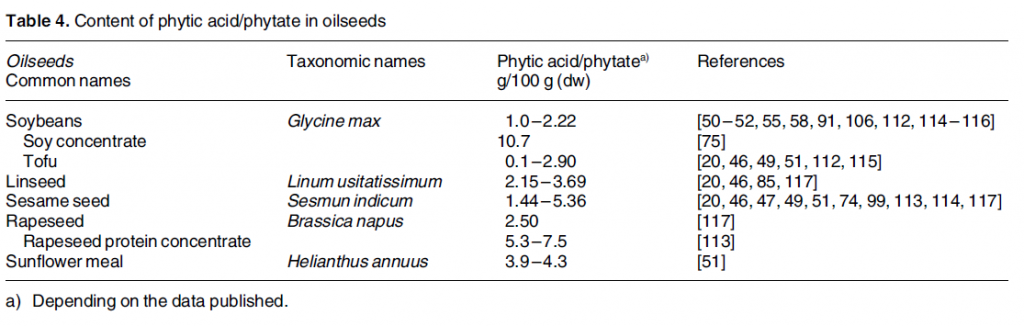
Phytic acid is phosphorus stores in nuts, edible seeds, beans/legumes, and grains. It is often referred to as anti-nutrient. Phytates (phytic acid) have been shown to decrease absorption of minerals, including iron, calcium, zinc and manganese. Phytates decrease the absorption by binding to the minerals before their uptake in the stomach and intestines. 5-10mg of phytic acid can decrease iron absorption by 50%. 1 This research done on non-WLS patients but is something to be aware of if you are having iron deficiency anemia or low calcium issues.
There are ways to combat the effects of phytic acid such as heat, soaking, fermenting, Vitamin C, protein, probiotics, and sprouting. 2
Phytic acid has many benefits such as preventing kidney stones, anti cancer effects, cardiovascular health protectant, binding with heavy metals and free radicals. It becomes an antioxidant and is a secondary messenger in cellular activity.
Phytate intake is something to be looked at if you are experiencing iron or calcium deficiencies.Adjusting your intake of phytates containing foods, combining them with high Vitamin C containing food items, and/or prepping them before consumption can decrease the mineral binding capacity. It would also be prudent to be aware of the timing between eating phytic acid containing foods and any vitamin or mineral supplementation.